About AHP
What is AHP?
Acute hepatic porphyria (AHP) is a group of rare genetic diseases that can cause severe, potentially life-threatening attacks and, for some, chronic symptoms that disrupt daily life.
There are 4 types of AHP
Most common
- Acute intermittent porphyria (AIP)
- Variegate porphyria (VP)
- Hereditary coproporphyria (HCP)
- ALAD-deficiency porphyria (ADP)
Extremely rare
Why AHP is often missed
Misdiagnosis is common, and people with AHP can wait years for an accurate and confirmed diagnosis. AHP symptoms can mimic gastrointestinal, gynecological, neurological, or mental health conditions—which may lead to years of misdiagnoses, unnecessary procedures, and hospital visits.
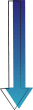
AHP can mimic other diseases: Know the signs and symptoms of AHP
Most people with AHP experience severe abdominal pain during attacks; other seemingly unrelated symptoms vary from person to person and change over time. Recognizing the symptoms is a crucial first step to help you and your doctor identify the disease and reduce the likelihood of attacks.
1Central nervous
system
Confusion
Anxiety
Seizures
Insomnia
Hallucinations
Depression
2Peripheral nervous
system
Limb weakness or pain
Numbness
Fatigue
Tiredness
Paralysis
Respiratory paralysis
Sensory loss
3Cardiovascular
Rapid heart rate
High blood pressure
4Cutaneous (skin)
symptoms*
Lesions or blisters on
5Gastrointestinal
Constipation or diarrhea
6Autonomic nervous
system
Unexplained abdominal pain
Pain in back or chest
Nausea and vomiting
Other
Dark or reddish urine
Low blood sodium
*Hereditary coproporphyria and variegate porphyria primarily.
The symptoms of AHP often resemble those of other diseases in the gastrointestinal, gynecological, and neurological or neuropsychiatric areas. Severe symptoms may lead to hospitalizations and unnecessary surgeries or procedures.
These are not all the possible signs and symptoms. Not everyone will experience the same ones—or with the same frequency or severity.
Understanding AHP: A Look Inside the Body
What AHP does to the body
1. It starts in the genes
People with AHP have a genetic defect that affects one step in the body’s heme-making process.
2. The liver can’t keep up
Your body relies on heme. But in AHP, one enzyme doesn’t work properly—especially when your body demands more heme. (This includes times of stress, fasting, or illness, or during the luteal phase.)
3. Toxins build up
When the system gets overwhelmed, toxic substances—delta-aminolevulinic acid (ALA) and porphobilinogen (PBG)—build up in the liver and spread through the body.
4. The nerves take the hit
These toxins are harmful to nerve cells and are associated with the painful, unpredictable symptoms of AHP.
5. What makes AHP so hard to find
Because it affects the nervous system, AHP can look like other diseases. That’s why it’s so often misdiagnosed.
By the time I was 14, I had more unexplained attacks. My symptoms included tremors, seizures, sunburns and light sensitivity, frequent vomiting, abdominal pain, severe all-body pain, muscle weakness, memory loss, and diarrhea.
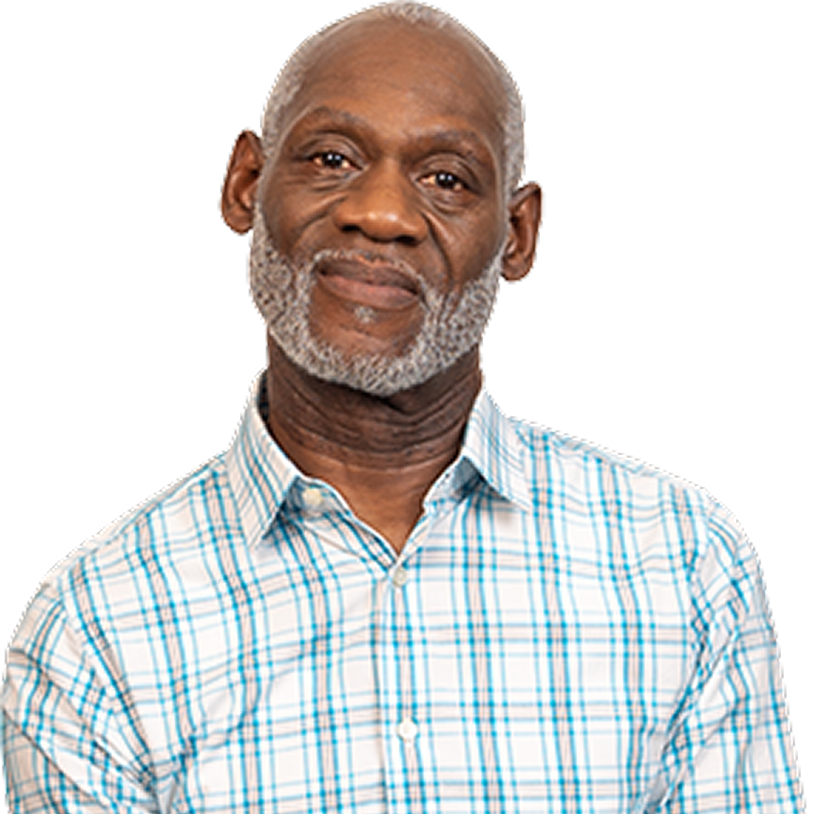
Everyone experiences AHP
in a different way
Acute attacks can be life-threatening and can last for days. Acute attacks are not the only sign of AHP—some people with AHP also experience debilitating symptoms daily, even when they are not having attacks. This is part of what makes diagnosis difficult.
Acute AHP attacks

Acute attacks can cause severe problems in many parts of the body, and often require hospitalization.
Chronic AHP symptoms

Chronic symptoms, such as anxiety, nausea, pain, and fatigue, can take a serious toll on some people with AHP.
AHP can affect anyone
Regardless of race, gender, or age—but it’s most commonly seen in women between 15 and 45. Around 80% of those diagnosed are women. Not everyone with the genetic mutation will develop symptoms.
There are tests your doctor can perform to help determine if you have AHP
AHP can be misdiagnosed as other conditions
The signs and symptoms of AHP can be mistaken for those of other conditions, shown below. These misdiagnoses can lead to unnecessary treatments, surgeries, and hospital stays.
Gastrointestinal disorders
- Irritable bowel syndrome (IBS)
- Acute gastroenteritis with vomiting
- Hepatitis
Neurological/neuropsychiatric disorders
- Fibromyalgia
- Guillain-Barré syndrome
- Psychosis
Gynecological disorder
- Endometriosis
Abdominal conditions requiring surgery
- Appendicitis
- Cholecystitis
- Peritonitis
- Intestinal occlusion
ALAD=delta-aminolevulinic acid dehydratase.